Orange County Traumatic Brain Injury Lawyer

TABLE OF CONTENTS
Traumatic Brain Injury (TBI) is extraordinarily common in California. According to the California Department of Public Health, California emergency rooms treated 142,139 people for traumatic brain injuries in 2007.
Of that, 29,354 were hospitalized, 7 percent of which died. The two leading causes for patients visiting the hospital with a traumatic brain injury are slip and falls and car accidents. A blow to the head or violent shaking of the brain within the skull can lead to a brain injury, both of which typically happen in slip and falls and car accidents.
These brain injuries can range from mild to severe. The most common type of brain injury in Orange County is a mild brain injury, also known as a concussion. Calling a brain injury “mild” is actually a misnomer though because they can be devastating for people and should be taken seriously. If you have recently sustained a brain injury due to someone else’s negligence, you may be entitled to compensation. Contact our Orange County traumatic brain injury attorneys at the Text Kevin Accident Attorneys to learn about how we can help you maximize your settlement. Call (888) 965-3827 for a free consultation with an Orange County personal injury attorney.
TABLE OF CONTENTS
What Is a Traumatic Brain Injury?
A traumatic brain injury (TBI) is defined by the CDC as a disruption in normal brain function as a result of a bump, blow, or jolt to the head. The severity of a TBI ranges from mild, moderate, to severe. A mild TBI is also known as a concussion.
How Do You Prove a Brain Injury?
Diagnosing a traumatic brain injury can be difficult because oftentimes the person does not show signs of physical injury, so they are often overlooked. A neurological exam is usually the first step, though. There are primarily two guidelines that are used, one published by the Department of Defense, and the other is called the Glasgow Coma Scale (GCS). If a TBI is suspected based on the results of these neurological exams, then brain imaging tests may be warranted.
Department of Defense Guidelines
The Department of Defense guidelines look at the duration of loss of consciousness (blacking out), post-traumatic amnesia (memory loss immediately following an injury), and altered mental status (confused or disoriented). Mild TBI/Concussion Mild concussion symptoms include:
- Loss of consciousness of fewer than 30 minutes; or
- Post-traumatic amnesia lasting less than 24 hours; or
- Altered mental status less than 24 hours. (Structural brain imaging is normal)
Moderate TBI Moderate brain injury signs are:
- Loss of consciousness for more than 30 minutes but less than 24 hours; or
- Post-traumatic amnesia lasting more than 24 hours but less than 7 days; or
- Altered mental status lasting more than 24 hours. (Structural brain imaging may be normal or abnormal)
Severe TBI Severe injuries to the brain include:
- Loss of consciousness for more than 24 hours; or
- Post-traumatic amnesia lasting more than 7 days; or
- Altered mental status lasting more than 24 hours. (Structural brain imaging may be normal or abnormal)
Glasgow Coma Scale (GCS)
The Glasgow Coma Scale is a 15-point test that assesses patients based on their ability to move their eyes and limbs and follow directions. Each of the three categories is given an individual score that is then added up all together:
Eye Response (4)
- No eye opening
- Eye opening to pain
- Eye opening to sound
- Eyes open spontaneously
Verbal Response (5)
- No verbal response
- Incomprehensible sounds
- Inappropriate words
- Confused
- Orientated
- No motor response
- Abnormal extension to pain
- Abnormal flexion to pain
- Withdrawal from pain
- Localizing pain
- Obeys commands
- Mild TBI/Concussion: GCS score of 13-15
- Mild TBI: GCS score of 9-12
- Severe TBI: GCS score of 3-8
Neuroimaging Tests
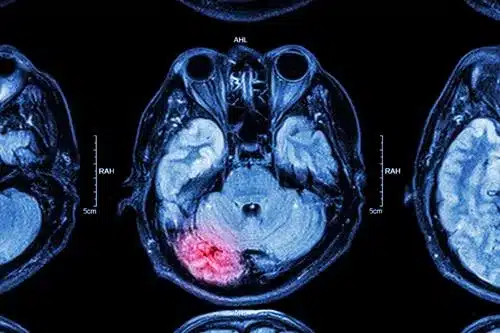
Neuroimaging tests may be warranted if an emergency room patient presents with symptoms of a TBI based on the results of a neurological exam. There are primarily two neuroimaging tests used to diagnose a TBI: (1) CT Scans, and (2) MRI.CT Scans
Computerized tomography (CT) scans are most commonly used by emergency room physicians who suspect a traumatic brain injury. A CT scanner uses a rotating X-ray machine to obtain images of brain tissue and brain structures. The scanners are capable of detecting blood clots (hematomas), brain bleed (hemorrhage), bruised brain tissue (contusion), and skull fractures. However, a CT scan will usually produce normal results for somebody with a mild TBI, such as a concussion.MRI
Magnetic resonance imaging (MRI) is most commonly used when symptoms persist following the acute period of a TBI. An MRI machine uses a magnetic field and radio waves to create images of your brain. These machines are particularly good at detecting injury to nerve fibers (diffuse axonal injury) according to the Journal of Affective Disorders. MRIs are also useful diagnostic tools as far as diagnosing a cerebral microbleed (microhemorrhage) and bruised brain tissue (contusion). It’s important to note that neuroimaging tests, such as CT scans and MRI, oftentimes show “normal” results. However, “normal” does not mean a person did not sustain a TBI. These tests typically only detect large abnormalities and fail to detect other signs of brain injury.What Are the Different Types of Brain Injuries?
The term “brain injury” can be vague because there are so many different types, and each type is associated with a different outcome. With that being said, brain injuries typically fall within one of three categories: (1) open head injury; (2) closed head injury; and (3) skull fracture.Open Head Injury
An open head injury, also known as a penetrating brain injury, occurs when an object pierces the skull and enters the brain tissue.Closed Head Injury
A closed head injury is a brain injury caused by an external impact that moves the brain within the skull but does not break the skull. A concussion is one type of closed head injury and the most common type we see from accidents in Orange County, CA.Concussion
A concussion is a brain injury that results in a temporary loss of normal brain function. Note, though, that a person doesn’t have to lose consciousness to sustain a concussion. A concussion is caused by either a blow to the head or a violent shaking of the head. Imaging studies, such as CT scans and MRIs, do not help diagnose a concussion; the diagnosis is clinical in nature.Epidural Hematoma (EDH)
An epidural hematoma refers to bleeding between the inside of the skull and the outer covering of the brain (called the dura). The leaking blood forms a hematoma (mass of blood) that puts pressure on the brain tissue.Subdural Hematoma (SDH)
A subdural hematoma refers to bleeding between the outer covering of the brain (dura) and the surface of the brain. The leaking blood forms a hematoma that puts pressure on the brain tissue.Intracerebral Hemorrhage (ICH)
An intracerebral hemorrhage refers to bleeding that occurs within the brain tissue.Cerebral Contusion
A cerebral contusion refers to a bruise on the brain’s surface, which causes bleeding and swelling inside the brain. In other words, a brain contusion often results in an intracerebral hemorrhage.Diffuse Axonal Injury (DAI)
A diffuse axonal injury refers to widespread damage of nerve axons throughout the brain, which disrupts nerve communication. Car accidents are the most common cause of DAI.
Skull Fracture
A skull fracture refers to a break in the skull bone. There are 3 types of skull fracture that are particularly relevant to accidents:
Linear Skull Fracture
A linear skull fracture refers to a break in the skull with a single fracture line. This is the most common type of skull fracture.
Depressed Skull Fracture
This refers to a fracture in the skull with pieces of bone being pushed inwards towards the brain.
Basilar Skull Fracture
A basilar fracture is located at the base of the skull. This is the most serious type of skull fracture.
Can You Get Brain Damage From a Car Accident?
You can absolutely get brain damage from a car accident. In fact, the CDC says that car accidents are the second leading cause of all TBI hospitalizations, only second behind falls. There are several other causes of brain injury as well, such as motorcycle crashes, bicycle crashes, and pedestrian accidents. As for car accidents, brain damage can happen in one of two ways: either from a direct blow to the head or from a violent movement of the head. Let’s take a look at both ways.
Coup-Contrecoup Injuries
A car crash can cause an occupant’s head to strike an object (e.g., dashboard, roof, steering wheel, or window) or an object to strike an occupant’s head (airbag, glass, or metal sheared from the car). This area of direct impact is called a “coup” injury. If the brain subsequently moves to the opposite side and strikes the skull again, it’s called a “contrecoup” injury. Coup-contrecoup injuries are responsible for every type of brain injury there is, including open head injuries and skull fractures.
Acceleration/Deceleration Injuries
A car crash can cause an occupant’s head to jerk backward and then forwards where it abruptly stops, meanwhile their brain still has forward momentum and winds up striking the inside of their skull. Acceleration/deceleration injuries are responsible for concussions, brain contusions, hemorrhages, and diffuse axonal injuries.
What Are Brain Damage Symptoms?
Symptoms of a brain injury might be noticed right away, or they might not appear at all until several days or weeks later. Sometimes people don’t even realize they are experiencing symptoms of a TBI until others bring it to their attention. TBI symptoms fall into one of these three categories: (1) cognitive, (2) emotional, and (3) physical.
Cognitive Symptoms
Decreased attention and concentration, difficulty processing and understanding information, language and communication problems, planning and organizing problems, problems learning and remembering new information, and problems with reasoning/problem solving/judgment.
Emotional Symptoms
Anger, anxiety or nervousness, depression, impulsiveness, mood swings, and irritability.
Physical Symptoms
Blurry vision, diminished sense of smell (anosmia), dizzy, fatigued, headaches, lethargy, nauseous, poor balance, poor coordination, reduced sense of taste, ringing in the ears (tinnitus), seizure, sensitivity to light (photophobia), sensitivity to sound (phonophobia), sleep disturbance, and vomiting.
These symptoms are a part of the normal recovery process for a brain injury. They can be expected to resolve within about 3 to 6 months for a majority of people.
Can TBI Symptoms Get Worse Over Time?
TBI symptoms can get worse over time, but how long those symptoms persist depends on the type of TBI you sustain. As you can probably imagine, people with a moderate or severe TBI can generally expect symptoms for a longer period of time than people with a mild TBI (i.e., a concussion).
Post-Concussion Syndrome
TBI symptoms do resolve fairly quickly for a majority of people who sustain a mild traumatic brain injury. However, for about 20% of people they don’t. When TBI symptoms continue to persist for months or years after an injury, it’s referred to as a post-concussion syndrome. According to the VA, a certain percentage of people with head injuries can be expected to experience the following symptoms of post-concussion syndrome at some point in their recovery:
- Sleep difficulties: 80 percent
- Poor concentration: 71 percent
- Irritability: 66 percent
- Fatigue: 65 percent
- Depression: 63 percent
- Memory problems: 59 percent
- Headaches: 59 percent
- Anxiety: 58 percent
- Trouble thinking: 57 percent
- Dizziness: 52 percent
- Blurry or double vision: 45 percent
- Sensitivity to bright light: 40 percent
These symptoms of post-concussion syndrome tend to gradually dissipate over time. Like any other injured body part, your brain needs time to heal itself through rest and relaxation. You wouldn’t go for a run the day after spraining your ankle, would you? The brain is no different. It also needs time to recover. People who give their brain sufficient time to rest before jumping back into their normal routine experience these symptoms for a shorter period of time than those who don’t. Rest assured, these symptoms will likely go away within 3 to 6 months without any formal treatment. If your symptoms are getting worse, this is a sign you need to cut back on your work and responsibilities so you’re under less stress.
Chronic Traumatic Encephalopathy (CTE)
CTE refers to a degenerative brain condition caused by repetitive mild traumatic brain injuries. According to the Concussion Legacy Foundation, a single mild TBI won’t necessarily cause CTE. Rather, evidence suggests that people with multiple mild traumatic brain injuries have a greater risk of developing CTE, which is a type of dementia. Repeated hits to the head cause a buildup of the protein called “tau,” which has been linked to the death of brain cells. Damage to brain cells that are necessary for healthy brain function causes neurological changes, such as: aggression, changes in personality, confusion, depression, difficulty with balance and movement, impulsive behavior, and memory loss. These symptoms of CTE may not appear until many years or decades later. And unfortunately, a definitive diagnosis of CTE can only be made after death during an autopsy. TBI symptoms can persist long-term, sometimes even life-long, for people who sustain a moderate or severe traumatic brain injury. These people may require extensive rehabilitation for persistent cognitive, emotional, and physical symptoms. Let’s take a look at some of the long-term consequences.
Dementia
Moderate to severe traumatic brain injuries are associated with an increased risk of developing dementia. Older adults who sustain a moderate TBI have a 2.3 times greater risk of developing Alzheimer’s disease, which is a type of dementia; those with a severe TBI have a 4.5 times greater risk according to the Alzheimer’s Association.
Seizures
Seizures occur when the brain has a sudden surge of electrical activity. These electrical disturbances in the brain can happen to 1 to 5 out of every 10 people who sustain a traumatic brain injury according to the Archives of Physical Medicine and Rehabilitation. The risk of having one of these seizures increases with the severity of the TBI. For example, seizures may affect as much as 50 percent of penetrating brain injury patients, 25-30 percent of severe TBI patients, and 5-10 percent mild to moderate TBI patients.
Mortality
Traumatic brain injuries are associated with increased mortality. People with a moderate to severe TBI who undergone inpatient rehabilitation are 2.2 times more likely to die as compared to the general population and have a reduced life expectancy of 6.6 years on average according to the Journal of Neurotrauma.
What Is the Best Treatment for Traumatic Brain Injuries?
Recovery from a traumatic brain injury varies quite a bit depending upon the severity of the injury. With that being said, every TBI patient will require rest so the brain can heal, and probably require medication to relieve headaches, like Neurontin.
Monitoring
If you sustain a TBI and go the emergency room, you won’t be discharged from the hospital until your condition has stabilized. In fact, you might even be admitted to Neurocritical Care, which is the ICU for people with a life-threatening brain injury. There are several devices that physicians will use to monitor the condition of your brain injury.
EEG Test
Surgery
Depending on the type of TBI you sustain, surgery may be necessary to relieve pressure on the brain caused by bleeding and swelling.Craniotomy
A craniotomy is used primarily to treat a hematoma putting pressure on the brain after head trauma. It involves removing a part of the skull called the bone flap in order to access the brain. Once the surgeon drains the hematoma using suction and irrigation, the bone flap back is secured back to the skull with plates and screws.Craniectomy
A craniectomy is preferred over a craniotomy when the swelling in the brain is significantly great. Just like a craniotomy, the surgeon removes a part of the skull called the bone flap to access the brain. But unlike a craniotomy, the surgeon doesn’t immediately secure the bone flap back to the skull. Instead, the bone flap is stored in a freezer for 1 to 3 months while the swelling in the brain continues to go down. Once the patient stabilizes, the surgeon performs a second surgery to secure the bone flap back to the skull again with plates and screws.Neuroplasticity
Luckily, the brain is capable of repairing itself by creating new brain cells to replace damaged ones. This ability of the brain to physiologically change and adapt after an injury is referred to as neuroplasticity. Neuroplasticity is at the heart of recovery from a brain injury, but it requires rest and time for the brain to create these new connections.Rehabilitation
Although the brain is remarkable in its ability to self-heal, therapy can help speed your recovery process along. You might undergo inpatient rehabilitation before you’re discharged from the hospital, or after you’ve been released, or both.Neuropsychology
A neuropsychologist is a licensed psychologist who administers tests that measure the degree of cognitive impairment caused by a brain injury. The results of this test will help guide treatment and rehabilitation for problems with behaviors, emotions, thinking, and memory.Occupational Therapy
An occupational therapist teaches TBI patients how to function in day-to-day activities, such as bathing, cooking, dressing, eating, grooming, home maintenance, toileting, and work.Physical Therapy
A physical therapist helps TBI patients improve balance, coordination, endurance, and strength so they can function at work and at home.Speech Therapy
A speech-language pathologist helps TBI patients improve language, speech, and swallowing skills so they can eventually return to work or school.Review Your Injury Claim With an Orange County Traumatic Brain Injury Attorney
As brain injury lawyers, we regularly represent the interests of victims who have been treated unfairly by an insurance company. We are committed to handling your brain injury claim from start to finish and will fight to make sure that you receive the money you deserve. If you have sustained a brain injury as a result of someone else’s negligence, contact the Text Kevin Accident Attorneys at (888) 965-3827 to schedule a free consultation.Kevin received both his bachelor’s degree and law degree from the University of California, Irvine. He is the managing partner of Text Kevin Accident Attorneys and is recognized as a standout in plaintiffs’ litigation for personal injury law by Best Lawyers, the oldest and most respected legal peer-review publisher. Kevin has written for several law magazines and is an award-winning car accident lawyer in California.
Orange County Practice Areas
Get started fast with tailored solutions for your accident claim
Car Accident
- Get support for your injury claim
- Secure compensation with proven success
- Strategize to win and maximize your value
Personal Injury
- Evaluate medical records for details and severity
- Negotiate settlements with insurance companies
- Represent clients in court for litigation
Truck Accident
- Investigate liability to determine fault
- Pursue maximum compensation from insurers
- Navigate complex regulations for successful claims
Motorcycle Accident
- Investigate causes to establish liability
- Pursue compensation from at-fault parties
- Navigate legal complexities for effective claims
Wrongful Death
- Establish liability in fatal accidents
- Pursue compensation for loss and suffering
- Navigate intricate legal paths for justice
Bicycle Accident
- Establish fault in bicycle collision investigations
- Pursue compensation for injuries and damages
- Navigate legal complexities for fair resolution
Catastrophic Injury
- Get a free consult for potential compensation
- Establish a robust legal strategy
- Pursue litigation avenues for your injury claim
Pedestrian Accident
- Rapid injury evaluation for pedestrian accident cases
- Swift and strategic legal support for victims
- Maximize compensation with proactive legal guidance
Brain Injury
- Maximize compensation for traumatic brain injuries
- Swiftly resolve cases for financial relief
- Experience compassionate guidance for your TBI
Spinal Cord Injury
- Optimize compensation for spinal cord injury victims
- Navigate legal intricacies with effective representation
- Offer empathetic support throughout your recovery
Uber Accident
- Drive your Uber accident claim to success
- Chart a clear route through insurance complexities
- Cruise through legal challenges with our support
Drunk Driving Accident
- Championing justice for DUI crash survivors
- Crafting powerful cases for injury compensation
- Hold responsible parties accountable for their actions
Hit and Run Accident
- Swift investigation of unidentified perpetrators
- Skillful navigation through complex legal processes
- Hold accountable those who flee the scene
More winning, less hassle with us
Transform car accident challenges into triumphs with our dedicated legal support.
- Get support for your injury claim
- Secure compensation with proven success
- Strategize to win and maximize your value

Kevin Crockett, Managing Partner
"Experience unity at our firm as I bring legal teams together for seamless collaboration and communication, ensuring successful navigation of car accident cases."
Answers, support, & solutions all in one place
Transform personal injury challenges into triumphs with our dedicated legal support.
- Evaluate medical records for details and severity
- Negotiate settlements with insurance companies
- Represent clients in court for litigation

Kelly Gales, Attorney
"Our legal team significantly accelerates personal injury claims, reducing delays when you choose us for your case."
The complete legal solution
Transform truck accident challenges into triumphs with our dedicated legal support.
- Investigate liability to determine fault
- Pursue maximum compensation from insurers
- Navigate complex regulations for successful claims

Kayla Johns, Case Manager
“At Text Kevin, we keep clients informed with crucial updates, paving the way for successful resolutions in every case we handle.”
Deliver results on time, all the time
Transform motorcycle accident challenges into triumphs with our dedicated legal support.
- Investigate causes to establish liability
- Pursue compensation from at-fault parties
- Navigate legal complexities for effective claims

Mike Buhler, Intake Manager
“Streamline communication with insurers and eliminate headaches when you partner with us for your injury claim.”
Succeed on claims with your team
Transform wrongful death challenges into triumphs with our dedicated legal support.
- Establish liability in fatal accidents
- Pursue compensation for loss and suffering
- Navigate intricate legal paths for justice

Helen Vu, Junior Case Manager
“You can easily share documents and photos with our team, and we’ll handle the rest for a seamless resolution of your case.”
Total commitment to guide you through
Transform bicycle accident challenges into triumphs with our dedicated legal support.
- Establish fault in bicycle collision investigations
- Pursue compensation for injuries and damages
- Navigate legal complexities for fair resolution

Ryan Gloudeman, Law Clerk
“With Text Kevin, you can regain lost hours managing claims yourself. We not only save you time, but expedite the process.”
Manage most any type of claim
Transform catastrophic injury challenges into triumphs with our dedicated legal support.
- Get a free consult for potential compensation
- Establish a robust legal strategy
- Pursue litigation avenues for your injury claim

Jonathan Haskett, Marketing Coordinator
“Stay connected throughout your case with quick and easy text communication, ensuring regular updates and timely alerts on the next steps.”
Forge results your way
Transform pedestrian accident challenges into triumphs with our dedicated legal support.
- Rapid injury evaluation for pedestrian accident cases
- Swift and strategic legal support for victims
- Maximize compensation with proactive legal guidance

Garrett Syke, Case Assistant
“We simplify your injury claim by organizing your case and narrating your story to the insurance company so you don’t have to.”
Never face legal battles alone again
Transform brain injury challenges into triumphs with our dedicated legal support.
- Maximize compensation for traumatic brain injuries
- Swiftly resolve cases for financial relief
- Experience compassionate guidance for your TBI

Kevin Crockett, Managing Partner
“We help visualize what results you want from your injury case and adjust our strategies to help you achieve it.”
Set your path to legal success
Transform spinal cord injury challenges into triumphs with our dedicated legal support.
- Optimize compensation for spinal cord injury victims
- Navigate legal intricacies with effective representation
- Offer empathetic support throughout your recovery

Craig Crockett, Partner
“Leverage our legal team to passionately advocate for you and witness us fight to achieve the results you’re looking for.”
Collaborate on solutions together
Transform Uber accident challenges into triumphs with our dedicated legal support.
- Drive your Uber accident claim to success
- Chart a clear route through insurance complexities
- Cruise through legal challenges with our support

Kelly Gales, Attorney
“Initiate and schedule meetings instantly with our legal team, ensuring prompt notifications on the progress of your case at every step.”
Lead your case to legal success
Transform DUI accident challenges into triumphs with our dedicated legal support.
- Championing justice for DUI crash survivors
- Crafting powerful cases for injury compensation
- Hold responsible parties accountable for their actions

Craig Crockett, Partner
"At Text Kevin, we value your time and expedite claim processes, providing efficient and exceptional service."
Teamwork makes claims work every time
Transform hit & run accident challenges into triumphs with our dedicated legal support.
- Swift investigation of unidentified perpetrators
- Skillful navigation through complex legal processes
- Hold accountable those who flee the scene

Mike Buhler, Intake Manager
“Here, we're all about teamwork, ensuring seamless collaboration among legal teams for successful case outcomes.”
Why Clients Love Text Kevin
Top-rated car accident lawyers recognized for excellence and trusted for maximum compensation in cases.

Million Dollar Advocates
Member
Rising Stars
2023
Ones To Watch
2024
Clients Love Us

Clients’ Choice
10.0
Attorney Of The Month
2021
Client Champion
2024

Curt Schultz
“Get an attorney like Kevin that is experienced and will actually manage your case. I was lucky to have found him”
Car Accident

Rick Werlin
“JUSTICE was served. Thank you for your knowledge and unwavering due diligence on my behalf!”
Pedestrian Accident

Jeffrey Marx
“Crockett and his team made my first car crash experience so much easier than I expected. Thanks team!”
Car Accident
Case Results
Explore our showcased victories in personal injury, where we turned challenges into triumphs for our clients.

$2.75M
Rideshare Driver
2020

$1.30M
Car Passenger
2023
$1.25M
Wheelchair Pedestrian
2019

$1.045M
Police Car Detainee
2023

Our California Offices
IRVINE
ANAHEIM
SANTA ANA
MORENO VALLEY
NORWALK
INDIO
PALM SPRINGS
Overview
Reviews
Photos
Services
About
Reviews
Services
- Car Accident Lawyer
- Personal Injury Lawyer
- Motorcycle Accident Lawyer
- Truck Accident Lawyer
- Wrongful Death Lawyer
- Slip and Fall Lawyer
- Dog Bite Lawyer
- Bicycle Accident Lawyer
- Pedestrian Accident Lawyer
- Traumatic Brain Injury Lawyer
- Uber Accident Lawyer
- Catastrophic Injury Lawyer
- Spinal Cord Injury Lawyer
- Burn Injury Lawyer
About
I'm Kevin Crockett, your Irvine based personal injury lawyer at Text Kevin Accident Attorneys. Specializing in various accidents, we secure victories for our clients with a proven track record. You only pay when we win. Serving Spanish speakers, we offer free 24/7 consultations for reliable legal support in Orange County.
Services
-
Free consult
-
Onsite services
Language
-
English fluent
-
Spanish fluent
-
Vietnamese fluent
Accessibility
-
Wheelchair accessible
Amenities
-
Restroom
-
Free parking
Crowd
-
LGBTQ+ friendly
Availability
-
Open 24 hrs.
Overview
Reviews
Photos
Services
About
Reviews
Services
About
I'm Kevin Crockett, your Anaheim based personal injury lawyer at Text Kevin Accident Attorneys. Specializing in various accidents, we secure victories for our clients with a proven track record. You only pay when we win. Serving Spanish speakers, we offer free 24/7 consultations for reliable legal support in Orange County.
Services
-
Free consult
-
Onsite services
Language
-
English fluent
-
Spanish fluent
-
Vietnamese fluent
Accessibility
-
Wheelchair accessible
Amenities
-
Restroom
-
Free parking
Crowd
-
LGBTQ+ friendly
Availability
-
Open 24 hrs.
Overview
Reviews
Photos
Services
About
Reviews
Services
- Car Accident Lawyer
- Personal Injury Lawyer
- Motorcycle Accident Lawyer
- Truck Accident Lawyer
- Wrongful Death Lawyer
- Slip and Fall Lawyer
- Dog Bite Lawyer
- Bicycle Accident Lawyer
- Pedestrian Accident Lawyer
- Traumatic Brain Injury Lawyer
- Uber Accident Lawyer
- Catastrophic Injury Lawyer
- Spinal Cord Injury Lawyer
- Burn Injury Lawyer
About
I'm Kevin Crockett, your Santa Ana based personal injury lawyer at Text Kevin Accident Attorneys. Specializing in various accidents, we secure victories for our clients with a proven track record. You only pay when we win. Serving Spanish speakers, we offer free 24/7 consultations for reliable legal support in Orange County.
Services
-
Free consult
-
Onsite services
Language
-
English fluent
-
Spanish fluent
-
Vietnamese fluent
Accessibility
-
Wheelchair accessible
Amenities
-
Restroom
-
Free parking
Crowd
-
LGBTQ+ friendly
Availability
-
Open 24 hrs.
Overview
Reviews
Photos
Services
About
Reviews
Services
- Car Accident Lawyer
- Personal Injury Lawyer
- Motorcycle Accident Lawyer
- Truck Accident Lawyer
- Wrongful Death Lawyer
- Slip and Fall Lawyer
- Dog Bite Lawyer
- Bicycle Accident Lawyer
- Pedestrian Accident Lawyer
- Traumatic Brain Injury Lawyer
- Uber Accident Lawyer
- Catastrophic Injury Lawyer
- Spinal Cord Injury Lawyer
- Burn Injury Lawyer
About
I'm Kevin Crockett, your Moreno Valley based personal injury lawyer at Text Kevin Accident Attorneys. Specializing in various accidents, we secure victories for our clients with a proven track record. You only pay when we win. Serving Spanish speakers, we offer free 24/7 consultations for reliable legal support in the Inland Empire.
Services
-
Free consult
-
Onsite services
Language
-
English fluent
-
Spanish fluent
-
Vietnamese fluent
Accessibility
-
Wheelchair accessible
Amenities
-
Restroom
-
Free parking
Crowd
-
LGBTQ+ friendly
Availability
-
Open 24 hrs.
Overview
Reviews
Photos
Services
About
Reviews
Services
About
I'm Kevin Crockett, your Norwalk based personal injury lawyer at Text Kevin Accident Attorneys. Specializing in various accidents, we secure victories for our clients with a proven track record. You only pay when we win. Serving Spanish speakers, we offer free 24/7 consultations for reliable legal support in Los Angeles County.
Services
-
Free consult
-
Onsite services
Language
-
English fluent
-
Spanish fluent
-
Vietnamese fluent
Accessibility
-
Wheelchair accessible
Amenities
-
Restroom
-
Free parking
Crowd
-
LGBTQ+ friendly
Availability
-
Open 24 hrs.
Overview
Reviews
Photos
Services
About
Reviews
Services
About
I'm Kevin Crockett, your Indio based personal injury lawyer at Text Kevin Accident Attorneys. Specializing in various accidents, we secure victories for our clients with a proven track record. You only pay when we win. Serving Spanish speakers, we offer free 24/7 consultations for reliable legal support in the Coachella Valley.
Services
-
Free consult
-
Onsite services
Language
-
English fluent
-
Spanish fluent
-
Vietnamese fluent
Accessibility
-
Wheelchair accessible
Amenities
-
Restroom
-
Free parking
Crowd
-
LGBTQ+ friendly
Availability
-
Open 24 hrs.
Overview
Reviews
Photos
Services
About
Reviews
Services
- Car Accident Lawyer
- Personal Injury Lawyer
- Motorcycle Accident Lawyer
- Truck Accident Lawyer
- Wrongful Death Lawyer
- Slip and Fall Lawyer
- Dog Bite Lawyer
- Bicycle Accident Lawyer
- Pedestrian Accident Lawyer
- Traumatic Brain Injury Lawyer
- Uber Accident Lawyer
- Catastrophic Injury Lawyer
- Spinal Cord Injury Lawyer
- Burn Injury Lawyer
About
I'm Kevin Crockett, your Palm Springs based personal injury lawyer at Text Kevin Accident Attorneys. Specializing in various accidents, we secure victories for our clients with a proven track record. You only pay when we win. Serving Spanish speakers, we offer free 24/7 consultations for reliable legal support in the Coachella Valley.
Services
-
Free consult
-
Onsite services
Language
-
English fluent
-
Spanish fluent
-
Vietnamese fluent
Accessibility
-
Wheelchair accessible
Amenities
-
Restroom
-
Free parking
Crowd
-
LGBTQ+ friendly
Availability
-
Open 24 hrs.
Get a FREE Case Review
100% Secure & Confidential